My Lab: The Cancer Biomarkers Team

My lab is the Histopathology section of a research team, led by Professor Johann de Bono, comprising six biomedical scientists and a pathologist. Our team is one of many in the Institute of Cancer Research (ICR). We oversee samples from cancer patients on clinical trials conducted within the Royal Marsden Hospital (RMH), where our patients are being cared for. The Vision Statements for the ICR and the RMH are “Making the discoveries that defeat cancer” and “Life demands excellence”.
Our clinical research team works alongside the ICR/RMH Drug Development Unit, where patients with advanced metastatic cancer participate in clinical trials, and the Prostate Cancer Targeted Therapy Group.
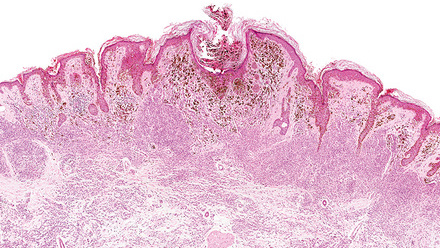
The Histopathology section has a wide range of skills including immunohistochemistry (IHC), immunofluorescence (IF), Fluorescence in situ Hybridisation (FISH) and digital pathology imaging, as well as array comparative genomic hybridization and next generation sequencing. We have also developed skills not traditionally considered to be histopathology based, including organoid culture and patient derived xenograft generation, as well as single cell and circulating tumour cell (CTC) analyses.
We work closely with pathologists evaluating all of our stained slides. This means assisting in identifying tumour in H&E slides, as well as scoring all the IHC, IF and FISH with pathologists.
Our lab is totally research based and we are passionate about our work, constantly investigating new biomarkers for cancer therapies and proteins of interest.
We have many collaborators worldwide including multiple US research partners and are part of the “International Prostate Cancer Dream Team” for Stand Up to Cancer. We work with many drug companies, and one of our major successes was the development and trial of the drug abiraterone (Zytiga) first synthesized and designed here in Sutton, Surrey, which is now widely used in the treatment of castration resistant prostate cancer and has been given to more than 300,000 men suffering from prostate cancer to date.
We are an academic institute and are actively encouraged to learn, read publications, attend courses and present our work. This means that we are easily able to gain knowledge for CPD. We are constantly striving to do the best for our patients, and a significant part of this is to publish articles on a regular basis.
As we in the Histopathology Team attend all of our biopsies, we have the privilege of meeting all our patients, and this brings into perspective why we are doing the work we do. As a result of attending these, we are able to assess the sample quality, working together to SOPs with doctors and radiologists, and know exactly what time the biopsy goes into formalin or is frozen, ensuring optimal sample processing with these being fixed or frozen immediately. This guarantees the best possible quality tumour tissue, and also excellent quality DNA and mRNA for next generation sequencing.
We make the most of all of our biopsies by cutting serial sections, as there can be numerous tests required from them. Who knows what biomarkers we will be expected to look for in future projects, which we are unaware of at present, but may become essential in our research and in our quest to find a cure for cancer?
Ruth Riisnaes is a Fellow of the IBMS and a Senior Scientific Officer and Laboratory Manager at the Institute of Cancer Research.