My Lab: The Donor Testing Laboratory

The Jack Copland Centre is the new award-winning building for the Scottish National Blood Transfusion Service (SNBTS). It is situated to the west of the dormant volcanic city of Edinburgh and is the national manufacturing centre for Scotland. Through the rotational doors, and multiple badge swipes, on the second floor you arrive at the donor testing laboratory. Donor testing is strictly regulated by the MHRA and is fully GMP compliant with every day-to-day task, ensuring the quality and safety of blood components and testing, on average, 650 samples per day. With each donation, three samples are collected – EDTA, serum and PPT. The SNBTS chooses to use EDTA for red cell serology, serum for virology screening and EDTA PPT for molecular testing and archive.
Each donation undergoes a series of mandatory and discretionary tests over different departments, which are situated at various locations in the open plan laboratory. All donors are confirmed for their ABO, RhD types, high titre and antibody screen. Automated phenotyping is performed (e.g. Fya, Fyb, M, S, etc.) plus manual phenotyping (e.g. Jka, Jkb, etc.) where appropriate, so that we can provide antigen-negative red cell units to patients who require specific blood components. In the virology section, where markers are analysed using a chemiluminescent assay, the mandatory markers tested are HIV, hepatitis C, HBsAg, HTLV and syphilis. Discretionary testing is performed for CMV and malaria. The molecular section uses two forms of PCR to test for mandatory markers. One analyser uses real-time PCR through a multiplex assay targeting HIV, hepatitis B and hepatitis C. A second platform is used to test for hepatitis E, using transcription-mediated PCR.
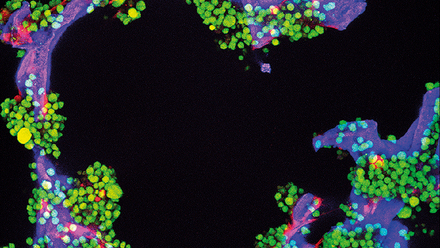
There are other testing platforms utilised to increase the safety of the blood supply. One example is the bacterial risk to platelet components. As platelets are stored at 22oC, this makes them an optimum environment for bacterial growth. Therefore, to check there is no bacterial contamination, 100% of platelet components have screening performed and monitored throughout their shelf life. Environmental monitoring is also carried out to provide assurance that components are manufactured in a sterile environment.
The QC section ensures manufactured components meet the required specification by performing a variety of tests, such as haematocrit, haemoglobin, and residual WBC on a percentage of components manufactured, as per “red book” – Guidelines for The Blood Transfusion Service.
SNBTS has added HbS screening of components, which are used for neonatal and sickle cell patients. Phenotyping is being expanded with more automated testing, which will ultimately result in the donor phenotype being permanently displayed on future red cell donations after confirmation.
Over the past three years, staff at SNBTS have overcome many obstacles. After transitioning from multiple sites, from more than one city and settling in the Jack Copland Centre we began to see the benefits of the national site.
Coronavirus has impacted the UK, yet at SNBTS we managed to maintain the integrity of the blood supply 24/7, 365. Throughout this difficult time, we still remain positive, achieving high standards and paving the way for a brighter and healthier Scotland.